Understanding Vulvar Cancer
Early Signs and Symptoms
Vulvar cancer is a rare form of cancer affecting the external female genitalia. Recognizing the early signs and symptoms is crucial for early detection and improved treatment outcomes. Some early symptoms may include persistent itching, burning, or soreness in the vulvar region. Women may also notice unusual bleeding, discharge, or changes in skin color or texture around their vulva.
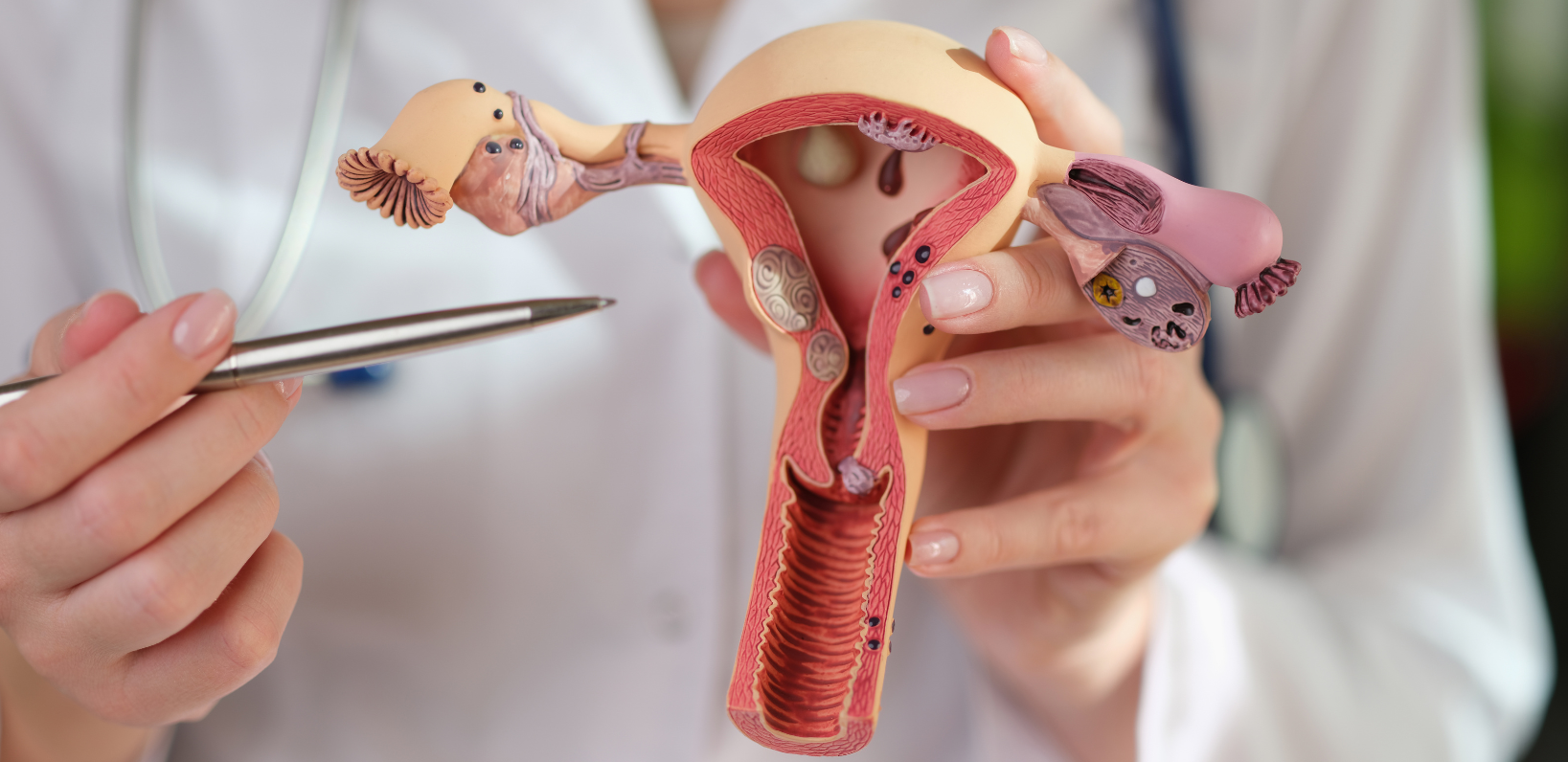
In some cases, the presence of a lump or growth in the vulvar area may be noticeable. It's important to consult a healthcare professional if you experience any of these symptoms or notice any unusual changes. Early detection can make a significant difference in the overall prognosis and survival rate of those affected by vulvar cancer.
Stages of Vulvar Cancer
The staging of vulvar cancer is a critical aspect of determining the appropriate treatment and assessing the prognosis. Vulvar cancer is typically categorized into four stages, ranging from Stage I to Stage IV:
- Stage I: The cancer is confined to the vulva or perineum and is no larger than 2 centimeters.
- Stage II: The cancer is larger than 2 centimeters but has not spread beyond the vulva or perineum.
- Stage III: The cancer has spread to nearby tissues such as the lower urethra, vagina, or anus, or lymph nodes have been affected.
- Stage IV: The cancer has spread to distant organs or has extensively spread through the regional structures.
Understanding the stage of vulvar cancer is imperative for determining the best treatment options and prognosis for the patient. Information on staging can also be found at the American Cancer Society.
Risk Factors
A myriad of risk factors can contribute to the development of vulvar cancer. Some of the most well-documented include:
- Age: The risk of vulvar cancer increases with age, with the majority of cases diagnosed in women over 50.
- Human Papillomavirus (HPV) Infection: HPV is a significant risk factor associated with vulvar cancer.
- Smoking: Tobacco use has been linked to an increased risk of vulvar cancer.
- Immunosuppression: A weakened immune system, whether due to medical conditions or medication, can increase susceptibility.
- History of Precancerous Conditions: Conditions such as Vulvar Intraepithelial Neoplasia (VIN) raise the risk of developing vulvar cancer.
Being aware of these risk factors can help in taking preventive measures and seeking medical guidance when necessary.
Treatment Options
The treatment of vulvar cancer typically involves a multidisciplinary approach that may include surgery, radiation therapy, and chemotherapy, depending on the cancer stage and other factors:
- Surgery: This is the most common treatment for vulvar cancer, with the goal of removing the tumor and some surrounding healthy tissue.
- Radiation Therapy: Often used in combination with surgery, radiation helps to destroy cancer cells and reduce the risk of recurrence.
- Chemotherapy: Applied in advanced stages or recurrent cases, chemotherapy involves using drugs to kill cancer cells.
Advanced treatment options may focus on targeted therapy or participation in clinical trials for cutting-edge treatments. Consulting with an oncologist who specializes in gynecological cancers can provide a treatment plan best suited to an individual's condition.
Conclusion
Early detection of vulvar cancer is pivotal for effective treatment and favorable outcomes. By remaining vigilant about observing early signs, understanding potential risk factors, and seeking timely medical attention, women can enhance their prognosis significantly. For more in-depth information on vulvar cancer, visit trusted resources such as the National Cancer Institute.

